A new study highlights the connection between socioeconomic factors and suicide rates. According to the study, unemployment, education inequality, and inadequate access to medical care were among the identified correlates of increased deaths by suicide.
The study, led by Shannon Lange at the Institute for Mental Health Policy Research in Ontario, Canada, was published in The Lancet Regional Health: Americas.
The research team examined two decades of data and identified several social and economic factors that played a role in the region’s suicide mortality rates. They write:
“Specifically, using 20 years of data, we identified the following contextual factors as having contributed to the suicide mortality rates in the region, namely: alcohol use, education inequality, health expenditure, homicide rate, intravenous drug use, number of employed medical doctors, population density, and unemployment rate.”
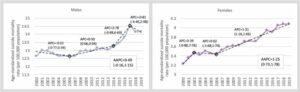 The age-standardized suicide mortality rate among males and females and the trend over time in the Region of the Americas, 2000–2019. Diamonds indicate identified points of inflection. AAPC: Average annual percent change; APC: Annual percent change.
The age-standardized suicide mortality rate among males and females and the trend over time in the Region of the Americas, 2000–2019. Diamonds indicate identified points of inflection. AAPC: Average annual percent change; APC: Annual percent change.
The researchers wanted to determine why the Americas (North, South, and Central America) have seen an increase in deaths by suicide over the past few decades while other parts of the world have experienced declining suicide mortality rates.
To conduct the study, they gathered the suicide mortality rates, by age and sex, for 33 countries in the Americas from 2000 to 2019. A wide variety of contextual factors were included in the analysis, taken from organizations like the World Bank and surveys like the Global Burden of Disease (GBD) Study. This allowed the researchers to compare changes over time while also looking at how different factors applied in other countries.
Low population density, high unemployment rate, and poor access to medical care were associated with increased suicide rates for both men and women. However, the researchers noted that suicide involves sociocultural factors that are impacted by sex and gender, so they also determined specific factors unique to men and women.1
For men only, suicide increased if there were more homicides and if alcohol and drug abuse was more prevalent. For women only, suicide was increased by higher rates of education inequality.
“Although most of the contextual factors identified seem relatively intuitive and are supported by the current literature,” the authors write, “the proportion of the country with a moderate population density is less so at first glance.”
“However, recently, Steelesmith et al. found that between 1999 and 2016, suicide rates were higher and increased more rapidly in rural than in large metropolitan US counties; suggesting that rural areas may be more sensitive to the impact of social deprivation than more metropolitan counties. Although increasing the population density of a country is not a realistic public health strategy for reducing the suicide mortality rate, improving social connectedness, and civic opportunities may be worth exploring as potential suicide prevention strategies.”
Current “suicide prevention” efforts are focused mainly on the individual and primarily involve delivering psychiatric treatment to those considered to be at risk. However, it is unclear how effective this strategy has been since suicide rates continue to increase despite significantly increased rates of mental health treatment in the United States.
In some cases, the very treatments that are delivered for suicide prevention may be causing more harm than good. For instance, antidepressants—often prescribed for even mild emotional distress in the United States—have been found to more than double suicide risk. Studies have also found that involuntary (forced) hospitalization—common for those expressing suicidal thoughts—leads to increased suicide and deters youth from reaching out in the future, too. And screening teenagers for depression doesn’t improve outcomes, either.
Although suicide is often viewed as being part of a theoretical neurobiological disease (like depression), the most consistent predictors of suicide are intense feelings of pain, hopelessness, and loneliness, which are the effects of many of the correlates found in this study—inequality, lack of medical care, low population density, unemployment, etc.
Thus, the researchers write that instead of focusing on the individual, the most effective means of suicide prevention is societal change:
“Multisectoral measures targeting health and social well-being in society, which are informed and developed using evidence on local contextual factors, should be emphasized in suicide prevention initiatives.”
****
Lange, S., Cayetano, C., Jiang, H., Tausch, A., & Oliveira e Souza, R. (2023). Contextual factors associated with country-level suicide mortality in the Americas, 2000–2019: a cross-sectional ecological study. The Lancet Regional Health: Americas, 20(100450). https://doi.org/10.1016/j.lana.2023.100450 (Link)
Editor’s Note: Part of MITUK’s core mission is to present a scientific critique of the existing paradigm of care. Each week we will be republishing Mad in America’s latest blog on the evidence supporting the need for radical change.
