A recent study published in Frontiers in Psychology suggests that adopting a Trauma-Informed Care (TIC) approach in inpatient psychiatric settings can significantly reduce self-harm and the use of seclusion and restraint.
The researchers, led by clinical psychologist Faye Nikopaschos, credit this reduction to weekly staff training on psychological stabilization and the use of the Power Threat Meaning Framework (PTMF). PTMF provides an alternative to the prevalent disease/diagnosis-centred approach in inpatient settings by focusing on the service users’ lived experiences.
Nikopaschos and her team state:
“Findings suggest that PTMF Team Formulation and Psychological Stabilisation training can contribute to significant reductions in self-harm and restrictive interventions (seclusion and restraint) on adult mental health wards.”
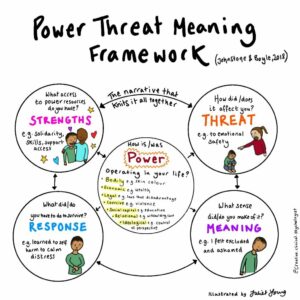
Illustration of the PTMF framework by psychologist Juliet Young (@Juliet_Young1)
The study aimed to assess the impact of TIC, applied through PTMF and staff psychological stabilization training, in an inpatient psychiatric facility. The team measured and compared the frequency of self-harm, seclusion, and restraint in a National Health Service adult acute inpatient mental health unit in London, both before and after the implementation of TIC. The data was gathered from two wards, starting with 23 and 22 service users and reducing to 18 in each over the study’s duration.
Data collection began in July 2017, prior to TIC’s introduction. The team introduced TIC in July 2018, and data gathering continued for the next four years until June 2022. They introduced two trauma-informed practices, PTMF team formulations and psychological stabilization training, to both wards in July 2018.
Two staff members conducted weekly PTMF formulations. Although service users were not physically present during these one-hour sessions, they were informed, asked for consent, and invited to guide the team on what to consider in the meetings. Service users received feedback after the meetings.
The researchers created a stabilization manual that guided the psychological stabilization training provided to the staff in each ward. The team engaged in weekly one-hour meetings to discuss topics such as self-compassion, soothing and safety, mindfulness, effective communication, breathing and relaxation, food and sleep, distraction and distancing, valued activities, grounding, and maintaining well-being.
During the five-year study period, there were 257 self-harm incidents, with 93 occurring in the year before TIC’s implementation and 164 in the four years following it. After introducing TIC, the monthly average of self-harm incidents decreased from 7.75 to 3.42, a reduction of 55.91%. Each year following TIC’s introduction saw a further decrease in self-harm incidents, ranging from 13.98% in the first year to 89.25% in the fourth year.
The study recorded 474 instances of seclusion, with 123 before TIC and 351 after. The average monthly seclusions decreased from 10.25 to 7.31 after TIC, a 22.66% reduction. The most significant decrease occurred in the second year after introducing TIC, with a 41.46% reduction. However, seclusions slightly increased in the third and fourth years due to staff shortages from COVID-19 but remained lower than pre-TIC levels.
The researchers noted 812 restraint instances throughout the study, with 193 occurring before TIC and 619 after. The average monthly use of restraints decreased by 19.82%, from 16.08 to 12.90, after TIC. Just like the seclusion data, the use of restraints was lowest in the first two years following TIC’s introduction but increased in the third year due to staff illness caused by COVID-19 and decreased again in the fourth year.
The authors acknowledged some limitations to their study. First, service users and medical staff were not involved in the initial design of the project. However, there are efforts to change this in the project’s ongoing development. Second, the medical staff was not involved in creating the interventions. Third, the absence of a control group means that the observed changes in self-harm, restraint, and seclusion cannot be definitively attributed to TIC. Finally, the reduction of inpatient beds over the research duration could have also influenced the results.
In conclusion, they stated:
“This service evaluation outlines a novel model of Trauma Informed Care (TIC), comprising Power Threat Meaning Framework (PTMF) Team Formulation and Psychological Stabilisation training. Findings suggest that the implementation of this model can contribute to significant and sustained reductions in incidents of self-harm, seclusion, and restraint in an adult inpatient mental health setting and highlight the benefits of TIC in this context.”
Researchers argue that understanding psychological distress requires addressing issues of power, as done in the PTMF. Past research has found that many psychologists are dissatisfied with the current focus on DSM diagnoses but are unfamiliar with alternatives like PTMF. Academics have also advocated for the use of PTMF in mental health nurse training.
However, some scholars warn that TIC approaches can be a guise for simply continuing diagnosis/disease-centred models in a language more appealing to service users. Additionally, others have argued that TIC risks re-traumatizing some service users.
In conclusion, this study provides compelling evidence of the potential benefits of implementing Trauma-Informed Care (TIC) in acute inpatient psychiatric settings. Utilizing the Power Threat Meaning Framework (PTMF) and staff psychological stabilization training appears to significantly reduce instances of self-harm, seclusion, and restraint.
Although some have raised concerns about the use of TIC, the dramatic decreases in harmful incidents within this study indicate a promising shift away from the traditional disease-centred approach. The authors call for further research and advocate for more extensive training in TIC and PTMF across psychiatric healthcare professionals, suggesting this as a viable and effective path toward improving patient care in mental health facilities.
****
Nikopaschos F, Burrell G, Clark J and Salgueiro A (2023) Trauma-Informed Care on mental health wards: the impact of Power Threat Meaning Framework Team Formulation and Psychological Stabilisation on self-harm and restrictive interventions. Frontiers in Psychology. 14:1145100. doi: 10.3389/fpsyg.2023.1145100 (Link)
This report was co-published with our friends and allies at Mad in America
