A Note on Language
This is an opinion piece on psychiatric drugs and why we may well be compounding mental health difficulties because of inappropriate prescribing. Firstly, however, it is important to make a point about the language used. For simplicity’s sake, I have used drug descriptions that many of us are familiar with; antidepressants, antipsychotics and anxiolytics. These names give the impression that the drugs are targeted medications that address or resolve an underlying specific disease or illness. This is all part of the myth and misinformation that surrounds this whole area of medicine. The ‘diseases’ or ‘disorders’ that these drugs are commonly used for are based on subjective lists of symptoms and/or behaviours. They are not based on an understanding of any underlying pathology and how it may differ between someone who receives a diagnosis and someone who does not.
In writing this blog, it is tempting to use the original names of the drugs, since these more accurately reflect the drug effects, rather than their supposed action against a ‘disease’ or ‘disorder’. The drugs we call antidepressants were known in the 1950s as ‘psychic energizers’ because it was observed that patients receiving iproniazid for tuberculosis experienced a lift in mood concurrent with treatment. Antipsychotic drugs are also known as neuroleptics (which means ‘nerve seizing’) or major tranquillisers and were first used for psychiatric patients in the early 1950s. After a dalliance with toxic and addictive barbiturates, benzodiazepines came along and were known as minor tranquillisers before being renamed anxiolytic (anxiety relieving) drugs. There are several classes of drug referred to an anxiolytic, but benzodiazepines are the most well-known.
It was in these early days that pharmaceutical researchers named these drugs as ‘anti’ to a disease that they were supposed to treat, in the hope that we may think of them as we do antibiotics or anti-inflammatory drugs.
So for the sake of simplicity, I have stuck with the standard nomenclature and dispensed with quote marks, but it is important to note that the names of these drugs probably owe as much to marketing departments as they do scientific laboratories.
Introduction
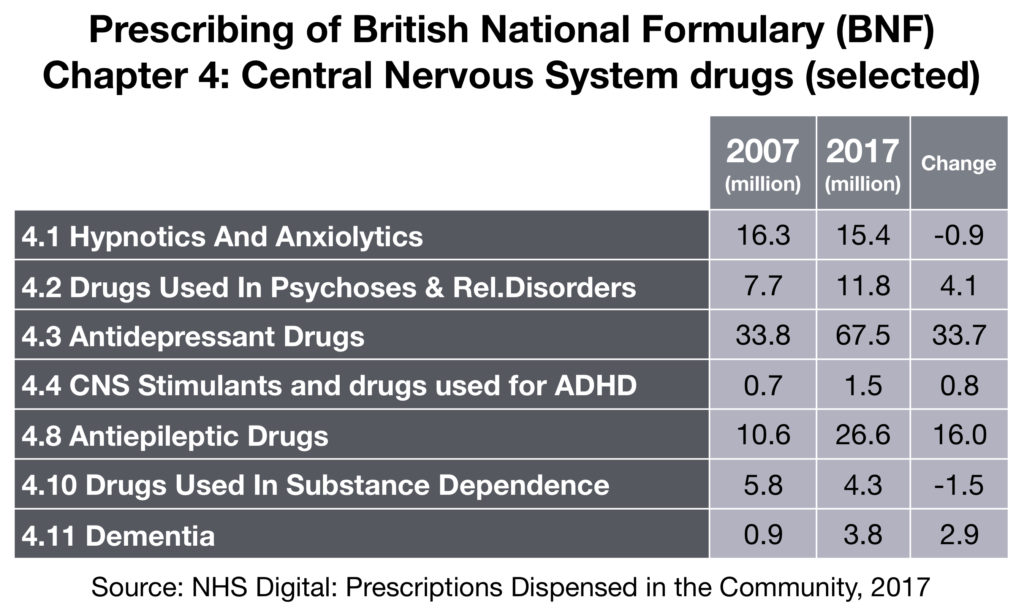
Psychiatric drugs are a global marketing phenomenon. In the US they are among the top ten most prescribed drugs, outpacing treatments for cardiac problems, cancer and high blood pressure. NHS digital report that in the UK, medication for high blood pressure is the most commonly prescribed item, followed by statins, indigestion remedies, painkillers and antidepressants. It reports that across drug groups, the greatest rise in 2016 was among antidepressants, with 3.7 million more items dispensed than in 2015, a six per cent rise. In 2017, UK doctors prescribed 67.5 million antidepressants in total.
Psychiatric drugs have entered the public consciousness like no other medications. They are written about in newspapers, discussed on chat shows, given cute names like Happy Pills or California Rocket Fuel. Should we be worried about the dramatic rise in prescribing? If 1 in 10 adults are on the drugs for extended periods, should we be concerned? What about when that figure inexorably creeps towards 1 in 5 or 1 in 2? Does it feel right that the number of children – some as young as five – being prescribed antipsychotics has doubled between and 2006 and 2011? Is it right that antidepressants have become a lifestyle accessory? Is it a good thing that we have normalized the conversation such that taking powerful, mood-affecting drugs is something we see as part of everyday life? Given the dramatic rise in prescribing are we all now mentally healthy, free to get on with our lives?
More and more patients, professionals, academics, authors and scientists are stepping forward in recent years to sound the alarm, yet we seem not to be listening. The situation we are in now is an unholy alliance between the marketing power of the pharmaceutical manufacturers and the cognitive dissonance of prescribers, who struggle with the notion that their treatments can be anything but beneficial. In short, the medical profession has no reason to change, no reason to come clean about the harm being done by casual and liberal prescribing.
It is time we took a stand as consumers since we cannot trust the evidence and science that the medical profession professes to rely on. We have bet the farm on the pharmacological revolution and we are losing that bet in spectacular style.
Why the Concern?
I’ve been taking an antidepressant for six years now, but in the last two years, I have come to feel that a grim future faces us unless we clamp down hard on the prescribing of psychiatric drugs.
For a treatment to be approved, I had previously assumed that it must be proven by the evidence that the benefit to the patient outweighs the risks. Recently, I have come to understand this is a popular misconception and that the onus is on us, as consumers receiving treatment, to review this evidence for ourselves and make a decision that is in our best interest. This is especially important for drugs that are taken for long periods, where damage may be compounded, and dependence may result.
We all know the horror stories about chemotherapy, the damage done to fast-growing cells like the hair follicles leading to hair loss and the stomach lining leading to relentless nausea and vomiting, yet we accept that to treat an aggressive cancer sometimes requires aggressive short-term therapy. Is the same true then of ‘mental disorders’ which we don’t understand, can’t explain and have never proven to be biological in origin? Are all those taking psychiatric drugs merely guinea pigs in a mass unlicensed clinical trial? Have we learned nothing from the rise and fall of barbiturates, which in retrospect given how toxic and addictive they are, seem like a very poor choice for mass market medications?
In short then, the concerns are:
- That psychiatric drugs are vastly overprescribed with no apparent decrease in suffering.
- That they come with serious adverse effects that are sometimes irreversible even when the medication is stopped.
- That they are not particularly effective.
- That they can lead to dependence and withdrawal symptoms in around half of those who take them.
- That the science and evidence supporting their use is biased and unreliable.
Let’s take each of these points in turn and let us also dispose of industry-sponsored evidence and trials in favour of the view of people who do not spend significant amounts of time at pharma-sponsored conferences and those who do not have extensive pharma share portfolios. Those brave people who have stepped away from the conventional wisdom and have willingly put themselves in the firing line. Why would they do that when it is so much easier, and probably considerably more lucrative, to toe the party line? What would motivate academics and psychiatrists to speak out against their own professional bodies or their colleagues, could it perhaps be the desire for the truth to be told?
As this is merely an opinion piece, the advice I would give to anyone interested in the facts and the reliable, unbiased science on these issues, is to read the following books:
- Anatomy of an Epidemic, Magic Bullets, Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America by Robert Whitaker.
- The Emperor’s New Drugs, Exploding the Antidepressant Myth by Irving Kirsch.
- A Straight-Talking Introduction to Psychiatric Drugs by Joanna Moncrieff.
- The Systematic Corruption of Global Mental Health: Book One: Prescribed Drug Dependence by Terry Lynch.
- Your Drug May Be Your Problem, How and Why to Stop Taking Psychiatric Medications by Peter Breggin.
- Pharmageddon by David Healy.
- Bad Pharma: How drug companies mislead doctors and harm patients by Ben Goldacre.
- Deadly Medicines and Organised Crime: How Big Pharma Has Corrupted Healthcare by Peter Gøtzsche.
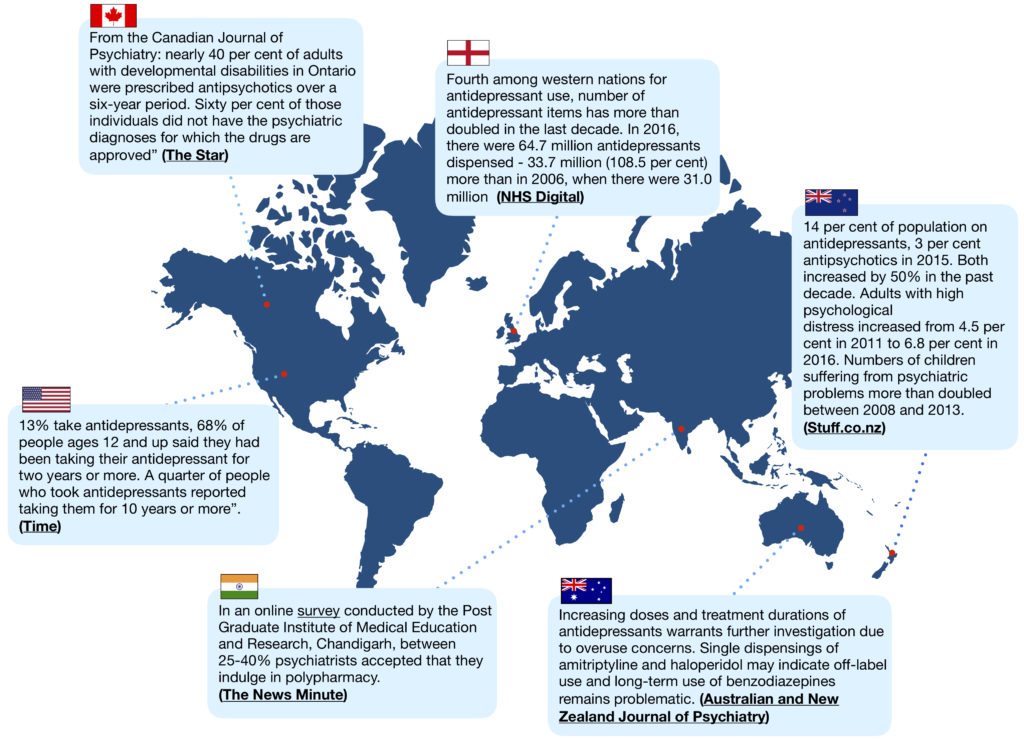
Prescribing Numbers
Messages alerting us to the dramatic rise in prescribing numbers have been given by the media, by celebrities, by academics and by psychiatrists. The World Health Organisation (WHO), Organisation for Economic Cooperation and Development (OECD) and US Centers for Disease Control and Prevention (CDC) have all sounded notes of caution. However, neither regulators, prescribers or patients seem to be listening because the trend has continued unabated and prescribing numbers continue to climb across the world. The numbers involved are shocking and concerning, yet the economic and social burden of ‘mental illness’ continues to rise.
There isn’t room enough in a blog such as this to go into detail about prescribing changes for antipsychotic, anxiolytic, sedative and stimulant drugs. Instead here is a flavour of the trends. In the British National Formulary, which is the prescribers bible, Chapter 4 represents Central Nervous System drugs including antidepressants, antipsychotics, anxiolytics, antiepileptics and sedatives. The total numbers prescribed have increased by 50% across the whole chapter between 2007 and 2017, from 138 million in 2007 to 208 million items in 2017. One may question why antiepileptic drugs are included here, but part of the reason for the increase shown is unapproved, off-label use of Gabapentin (Neurontin) for bipolar disorder and ADHD, which itself was the subject of a 2003 lawsuit, settled for $430 million.
Recently we have also seen evidence of an international effort to boost prescribing numbers for benzodiazepines, even though many prescribers are more aware of the need for short-term prescribing than they are in the case of antidepressants.
Antidepressants may be the visible ‘poster child’ of psychiatric prescribing, but increases are being felt in many classes, yet the science supporting such increases is proving very difficult to find. The main reason given in interviews with prominent psychiatrists and doctors is “more people seeking help”.
Adverse Effects
Have you ever actually read the Patient Information Leaflet that comes with your drugs? Some have, many won’t for fear of being frightened. At first reading, you may feel it is a comprehensive listing of effects with reassuringly small percentages of those potentially affected. However, since most clinical trials obtain results after a short treatment period (eight weeks in the case of the largest ever antidepressant meta-analysis) is it not then safe to assume that the reports of adverse effects are similarly based on short-term reporting only? Does the leaflet indicate over what time period you may experience certain symptoms? If not, perhaps it should, in order to help us all make an informed choice. For example, how would you feel if the leaflet said you have a significant chance of permanent sexual dysfunction after taking an SSRI antidepressant? Or a high chance of being affected by tardive dyskinesia in the case of an antipsychotic, or interdose withdrawal and protracted withdrawal syndrome from a benzodiazepine? In particular, you may want to pay close attention to the section labelled “frequency unknown” as these adverse effects seem to crop up far more readily than we have been led to believe.
A swift Google search of drug company settlements tells us something significant. The pharmaceutical manufacturers preference is to spend millions of dollars in settlements to suppress the message that the drugs could be dangerous. If they had evidence that proved beyond doubt that the drugs were safe, would they not then fight each trial to conclusion?
Efficacy
If you lived in the UK, on the morning of February 22, 2018, you would have woken to a media circus, proclaiming as loudly as it could that the debate about antidepressants ‘working or not’had finally been ended. The media were reporting on the largest ever comparative antidepressant meta-analysis, which reviewed the results of 522 placebo-controlled trials of 21 different antidepressant drugs. Did this study really end the debate? Now the media hype has rolled on by, we can answer that question. If you read the study itself, you can clearly see that results were taken at eight weeks, or as close to eight weeks as possible. Even then, when the scientists running the trials picked the point in time which showed the drug in the best possible light and best suited their desire to tell a positive story, the conclusion is that certain antidepressants might be ever so slightly better at reducing symptoms than a placebo at 8 weeks. Hardly earth-shattering news then. What is more, the authors themselves were honest about the modest conclusions reached, writing:
“We found that all antidepressants included in the meta-analysis were more efficacious than placebo in adults with major depressive disorder and the summary effect sizes were mostly modest. It should also be noted that some of the adverse effects of antidepressants occur over a prolonged period, meaning that positive results need to be taken with great caution, because the trials in this network meta-analysis were of short duration.”
How did this modest appraisal be amplified to the status of a clarion call to the UK population? Perhaps this Press Release from the Science Media Centre tells us what we need to know.
It seems clear that a great deal of effort and time went into this meta-analysis, which is time and effort that could have been saved because this large, exhaustive study confirmed the conclusions reached by Professor Irving Kirsch more than ten years ago.
If psychiatrists really wanted to help us with the minimum possible harm, they would consider prescribing a placebo. Many people would experience near the same level of relief when compared with the active drug (as demonstrated in the Lancet meta-analysis) but they would be exposed to less severe adverse effects and the potential for dependence would be minimized. Psychiatry may claim it to be unethical to knowingly prescribe a drug with no active ingredient, but I argue it is unethical to prescribe psychotropic drugs without a balanced and realistic assessment of the potential for harm, weighed up against the chance of benefit. Prescribing placebos, even with full patient knowledge, is already under investigation and showing great potential, this is not myth, it is simply harnessing the human body’s incredible powers of healing when given the correct stimulus.
Dependence and Withdrawal
In April 2018, the New York Times ran an article recounting the experiences of people who had tried to stop taking their antidepressant drugs. Shortly after the article was published, the comments section saw a huge influx of people recounting their awful experiences and over 8,800 people wrote in to share their stories. If you take time to read many of the comments, a theme emerges and that is one of professional medical denial. In many cases, people report that their experiences were discounted by their doctors, or even worse they were given such poor-quality withdrawal advice that they became very ill as a result. Some commenters reported that these difficulties were then further dismissed, leading to accusations of attention seeking or being labelled with some medically unexplained somatic or functional disorder (for which ironically the suggested treatment includes antidepressant medications).
As the New York Times noted in its article, something is going on here that is remote from the medical understanding of the effects of long-term treatment with psychiatric drugs. Psychiatry itself has been slow to respond, but there are some professionals writing about the issue, with US-based psychiatrist Doctor Josef Witt-Doerring and co-authors writing about the huge efforts that go on in online support forums like Surviving Antidepressants and Benzo Buddies. Clearly then, the users of these drugs have been forced to self-support because the response of the medical community has been woeful. General doctors and psychiatrists often lack any knowledge of how to help people withdraw, preferring to give non-evidence-based advice, such as that found in the NICE Pathways Guidelines on antidepressant treatment in adults, in which it is written:
Stopping or reducing antidepressants
Advise people that discontinuation symptoms may occur on stopping, missing doses or, occasionally, reducing the dose of the drug. Explain that these are usually mild and self-limiting over about 1 week, but can be severe, particularly if the drug is stopped abruptly.
Normally, gradually reduce the dose over 4 weeks (this is not necessary with fluoxetine). Reduce the dose over longer periods for drugs with a shorter half-life (for example, paroxetine and venlafaxine).
Advise the person to see their practitioner if they experience significant discontinuation symptoms. If symptoms occur:
- monitor them and reassure the person if symptoms are mild
- consider reintroducing the original antidepressant at the dose that was effective (or another antidepressant with a longer half-life from the same class) if symptoms are severe, and reduce the dose gradually while monitoring symptoms.
Nowhere in this paragraph is there a single reference to a study or observational account that we can use to assess the evidence supporting this view. Not only that, the advice given is so generic as to be less than helpful either for doctor or patient. For example, precisely how does one “gradually reduce the dose over 4 weeks”? This is not possible using conventional standard registered dosages, so the doctor has no alternative but to give advice that the patient cannot follow irrespective of how much they would like to. I believe this lack of clarity, the lack of evidence and the reliance on guesswork and anecdotal experience risks failing both patients and doctors alike.
There has been recent action in the UK that starkly highlights the effects of this lack of clarity and paucity of evidence. In February 2018, a group of thirty academics, psychiatrists and people with lived experience, including myself, clashed head-on with the Royal College of Psychiatrists specifically about antidepressant withdrawal. As recounted in detail elsewhere, senior members of the Royal College in responding to criticism of antidepressants, made a public statement in The Times newspaper:
“We know that in the vast majority of patients, any unpleasant symptoms experienced on discontinuing antidepressants have resolved within two weeks of stopping treatment”
It is important to note that the Royal College had previously undertaken their own survey, showing that 63% of respondents reported withdrawal symptoms. This survey, which, following a formal complaint, was removed from their website, said this about the duration of withdrawal effects:
“People in our survey reported that the symptoms generally lasted for up to 6 weeks. A small percentage of symptoms lasted longer than this. A quarter of our group reported anxiety lasting more than 12 weeks.”
Furthermore, the largest direct-to-consumer survey of antidepressant users to date found that 27% of 1,521 users in New Zealand experienced antidepressants to be addictive. More than half (55%) reported withdrawal symptoms and 46% of those described the withdrawal symptoms as ‘severe’ (Read et al., 2014). So, who is correct, those with a vested in interest in downplaying concerns with the drugs, or people who only seek recognition of, and support with their struggles?
The complaint against the Royal College remains an ongoing concern, but if you would like to see some of the responses to the Royal College’s two-week statement first hand, you need only search Twitter using the hashtag #MoreThan2Weeks.
As a final point, language here is equally important and correct descriptions of this matter hugely. The term ‘discontinuation syndrome’ has entered the lexicon of vague terminology that seems de rigeur for the medical assessment of mental health difficulties. This obfuscating term is more about protecting doctors’ interests than it is about recognizing the hell that many people describe as they are forced to reduce agonisingly slowly to try and stave off the worst of the withdrawal effects. In 2012, Peter Gøtzsche, Director of the Nordic Cochrane Centre, one of the world’s most prestigious research institutions, and co-authors, after reviewing and comparing papers reporting withdrawal effects from benzodiazepines and SSRI antidepressants wrote:
“Withdrawal reactions to selective serotonin re-uptake inhibitors appear to be similar to those for benzodiazepines; referring to these reactions as part of a dependence syndrome in the case of benzodiazepines, but not selective serotonin re-uptake inhibitors, does not seem rational.”
Biased, Industry-sponsored Trials
It is fitting that many entire books have been written on this subject because it is a broad, complex and utterly bewildering area of medicine. As a non-expert, I don’t have the experience, wit or wherewithal to concisely recount the tricks, shortcuts, underhand practices and downright dishonesty that goes on in trials of psychiatric drugs. The best quote I have ever heard on this comes directly from Robert Whitaker, science writer and journalist, who himself once ran a company reporting on clinical trials. In relation to randomised controlled trials of psychiatric drugs, he said to me “these studies are designed in such a way as to tell a story that will make that drug successful in the marketplace”. Does this sound to you like an approach that will generate the safest, most cautious approach for the consumer?
Recently, you may well have heard psychiatrists and researchers wringing their hands and telling us “there is no research into new psychiatric drugs”. Quite often they decry the criticism of the drugs and the fact that pharmaceuticals aren’t making money any more from psychiatric prescribing because most, if not all drugs are now off patent and can be manufactured, under license, as generic medications. The last time I saw any kind of licensing agreement, significant sums of money were involved for the licensee and I don’t hear pharmaceuticals very often issuing profit warnings. So, I have little sympathy because the fault here lies with the pharmaceutical manufacturers themselves, they have saturated every market they can access, played fast and loose with the science and been held to account in courts of law. To then exit a particular market because of such behaviour seems motivated not by concern for patient safety. As an aside, here is an interesting piece on the costs of setting up your own generic pharmaceutical manufacturing business.
Demonstrating our Power as Consumers
Deciding to take a psychiatric drug is one of the most important decisions you will ever take. Faced with a decision of this magnitude it pays the smart consumer to know the facts and be prepared. These drugs are not proven to be safe or effective, despite what psychiatry tells us and taking them should be approached with caution. Furthermore, the particular drug that it is recommended you take and at what dosage is not evidence-based, those decisions are based on conjecture, observation, a feeling the doctor has. Is that sufficient for you to feel comfortable that your safety as a patient is paramount?
If your doctor prescribes you a psychiatric drug and you go back for your check in at eight weeks, ask your doctor to prove to you using the evidence that there is benefit in you taking the drug for longer periods. They must have based the decision to medicate you on evidence, so make a polite and reasonable request to see that evidence. They will struggle, because the high-profile studies, like the recent Lancet antidepressant meta-analysis, are fundamentally flawed, taking their results at eight weeks, totally out of step with how these drugs are prescribed. If you take the drugs for longer than eight weeks, you are in uncharted territory as far as the clinical trial evidence is concerned. If studies exist that prove beyond doubt that the drugs are safe over years and years of use, let’s see them. Could there be a reason why psychiatry redirects and avoids answering the key question for anyone struggling with their mental health: are the drugs safe for long-term use? If there were studies proving this, surely psychiatry would have been shouting the results from the rooftops, instead, we are met with deafening silence on the matter.
What you may well find then, is that your doctor or psychiatrist falls back on the old reliable “in my clinical experience” argument, claiming that they have seen hundreds of patients benefit with no ill effects or problems coming off the drugs. Well, I’m sorry dear doctor, one cannot have one’s metaphorical cake and eat it too, that is not how evidence-based medicine works. Show me the clinical trials and please excuse me if I am not totally reassured by your opinion, no matter how well-intentioned that may be. My long-term physical and mental health and wellbeing could well be at stake.
Many academics, mental health professionals and doctors feel that mental health is a social issue that requires social interventions. Psychiatric drugs can’t address isolation, poverty, inequality, racism, intolerance, hatred, bigotry, sexism, etc., but they can mask those things. Perhaps that is why they are so successful. The blame is placed on us, the patient, for being broken because it obviates the need for powers that be to take any action to address those underlying causes of distress and suffering.
I argue that the power is in the hands of the well-informed consumer and that psychiatric drugs should be treated like any other commodity. We should coldly and from a distance weigh up the pros and cons and consult a wide range of views and sources before making a decision that we feel is in our best interest. For some, that will still be medication but hopefully based on a decision that is fully informed and not coerced or made because of myths and half-truths.
Six years ago, I would have welcomed the chance to make an informed choice and an informed decision about treatment. I was weak, fatigued and vulnerable being utterly and completely in the frigid embrace of depression, consumed by fear and lacking the mental facility to question what I was being told. I was coerced and led on a merry dance, ultimately to the detriment of my health, my confidence, my family and my social life.
You deciding to take drugs for a mental health problem is YOUR decision, not mine, not your doctors. Treatment decisions require careful judgement and the help of an impartial supporter. Finding an impartial supporter is difficult but not impossible and could immeasurably improve your long-term outlook. There are no certainties where ‘mental illness’ is concerned and that applies equally to the medications we often use in response.
If you are currently taking psychiatric drugs and you decide they are not for and you wish to stop, please do so slowly and sensibly, preferably with the help and support of an experienced practitioner who has successfully withdrawn people from their drugs previously. If finding someone face to face is too difficult, there are excellent and reliable online resources like the Inner Compass Initiative, Surviving Antidepressants, Benzo Buddies and Mad in America’s Provider Directory to name a few.
Finally, in every piece on this subject that I have ever read, there is a section dedicated to apologising for having views that are contentious. I will not do that. Instead, I say that your suffering is real, the cause is contested, and the recommended treatment could be harmful if relied upon for longer than necessary. The choice, as they say, is yours, but when you do make that choice, make it an informed one.




Hi James, we all now know what we wish we would of known before we didn’t know it, alas our only hope is now to get this information out to the general public so others don’t suffer as we have. The internet wasn’t around when I was young and I was given a pill I thought was for an ear infection. That was the spoke in the wheel that broke the whole bicycle where my health was concerned. Then 30 years of suffering and how I am still alive I am not sure. The NHS has much to learn to evolve to actually go from harming people to helping them but reluctance to learn and people paid lots of money to hold up the house of cards is going to take some blowing down, but I feel positive. I have too. As the darkness is all around.Take care.
There is a testable, verifiable and proven drug treatment for some psychiatric illnesses. One in which there is a blood test, a known mechanism of action and verifiable cure. It is standard anti-biotics in the treatment of infection such as Lyme disease, syphilis et al. The neuro-psychiatric manifestations of these infections are misdiagnosed as mental illnesses. On the basis that we are looking for “evidence based” treatments (shocking to lay persons that all treatments are not evidenced based btw) and that in a recent study 30% of prisoners (patients) in a psych ward tested positive for one of these infections, and the fact that anti biotics are the ONLY medication to ever cure psychiatric issues, they should be the first and only treatment for all psychiatric and psychological problems. As the “compounds prescribed for depression” act no better than placebo and “compounds prescribed for psychosis” are deadly lobotomy inducing poisons, a short course of antibiotics would also “cure” non infection created psychological issues by way of placebo in depression and letting nature heal in psychosis. It would be in the public interest to allow drug companies to charge a fortune for these simple drugs and extend patents on antibiotics to 100 years. This way they won’t feel the need to invent illnesses to suit any dangerous compounds that they accidentally come across in the lab, bribe and corrupt a branch of “medical” professionals, commit manslaughter by fraud etc etc.
Dr Neil
your comment does not seem to address the subject of the blog apart from the link.
I may look at the link but I may not, having a life n all.
Hey ho.
James
Thank you for writing this very comprehensive piece which describes very well the situation that patients are finding themselves in now.
Whilst academic debates are raging fiercely all around us, the fate of actual patients seems to be completely forgotten – or, as we are finding out to our horror, real patient evidence just completely ignored and airbrushed from ‘the evidence’ of so-called Evidence-Based medicine. Surely the struggling patients – and the inexorably rising levels of disability and suicides – are ‘the evidence’! If people ‘got better’ with the treatments they would no longer ‘show up’ in the mental health statistics! Instead the mental and physical health statistics are revealing very alarming evidence …. that the most commonly prescribed medicines are making many people extremely ill – mentally and physically. Killing them quickly or slowly. And no one wants to know. Our Scottish and Welsh public petitions are revealing very disturbing ‘evidence’…
Dear Recoveryrenewal, thank you for reading and for your comments too. It really is time that we had an honest and open debate about the use of psychotropic drugs for psychological distress. As you say, the lived experience voice must be paramount in that debate. The Scottish and Welsh petitions that you refer to are doing a huge public service in bringing the patient voice before the ‘powers that be’ so they can read the experiences related so powerfully and ask themselves the questions that we have been asking ourselves for some time.
James,
Sincere thanks and congratulations on the launch of MAD IN THE UK.
Your introductory blog is outstanding.
It is a sophisticated and genuinely evidence-based review of the real issues facing those exposed to psychotropic drugs.
In addition to prescriber denial, and rejection of the severity and duration of withdrawal syndromes from SSRI/s (and other classes of psycho-active prescribed drugs) the lack of prescriber awareness of the prevalence and severity of AKATHISIA is a matter of profound concern.
It would appear that prescribers of SSRIs/SNRIs and other akathisia inducing drugs have limited training in, and limited understanding of this life threatening and most serious adverse drug reaction (ADR).
It remains poorly understood, or indeed denied by prescribers, that akathisia causes suicidality and completed suicide.
The prescriber has duty to know of, and understand the ADRs of the “medications” that he/she prescribes.
They do not, and our children (and many adults) pay a terrible price for this professional failure.
Because of prescriber ignorance of akathisia it is vulnerable to misdiagnosis as “Emergent Serious Mental Illness” (SMI) and the poisoned patient is likely to be incarcerated and forced to ingest more of the akathisia inducing drugs.
The resulting injuries destroy lives.
This is an intolerable denial and/or ignorance.
There appears to be immunity from from medico-legal accountability.
The families of those killed, and those who are terribly injured have no access to compensation.
Dear Retired Physician, thank you for reading and for taking the time to comment. I agree that akathisia is a poorly understood, little discussed but serious issue that needs to be brought into the open and discussed properly. I hope that we can cover this most grave of ADRs in future writings on the site. In the meantime thank you so much for your thoughts and feedback.
James…a pleasure to make the first comment on your first substantial MITUK piece! It’s well written.
Good to see the recommendation of Ben Goldacre’s Bad Pharma, and I have a lot of time for Robert Whitaker’s work (by no means have I read all of it though).
Today I am very busy too: taking on the less well-known links between overmedication and anti-diagnosis that I have repeatedly brought to your attention since May: https://drnmblog.wordpress.com/2018/09/06/complaint-to-maudsley-hospital-governors
I will make just one point now. You write that six years ago you were ‘weak, fatigued and vulnerable being utterly and completely in the frigid embrace of depression, consumed by fear and lacking the mental facility to question what I was being told.’
Under ‘topics’ at the right here, ‘psychology’ has just one linked piece: to your interview with the lead author of the ‘Power Threat Meaning Framework’. According to the PTMF, diagnoses of mental disorders are to be abolished, to be replaced by a single quasi-diagnosis (my term, I have to be brief) of ‘Complex PTSD’ (search the 400+ page long version for that phrase). That means that in your ‘vulnerable’ state of ‘depression’, if you can’t remember sufficient traumas, in order to access support you might feel under pressure to make them up. Are you happy with that?
James, good luck, but I suggest you need to use words such as ‘unbiased’ with more care. Best wishes.
Dear Neil, thank you for commenting. As noted in our guidelines, the MITUK collective is committed to debate that is respectful and accurate. We would therefore like to point out that the PTM Framework does not propose replacing existing diagnoses with a single category of ‘Complex Trauma’. The second part of your comment makes unfounded allegations against a clinical psychologist, and after discussion within the moderating team we have therefore decided to delete this part of your comment. The MITUK Collective.